HCVME 2023 Review, Each Year, I’m going to add to this story, little by little, to keep you updated on my journey from diagnosis to transplant to treatment, to helping eliminate Hepatitis C.
It was a hot summer day in late July of 1999; Y2 K was the biggest concern on anyone’s mind, but I was 12, my concerns lay in how much pizza I could get from the pizza party coming up that Friday. I was in Tennis camp, and while I wasn’t great at Tennis, I was great at eating pizza. It was still a few days away, and like most 12-year-olds, I’d drink Gatorade and sodas in between the class sessions. But when my dad picked me up that day, I had little clue about how much all of our lives would change from such a small series of events. Upon arriving home, I rushed to the bathroom. The color was unusual, a dark, iced-tea colored urine; alarmed, I called over my dad. Upon his inspection, we decided a visit to the doctor was in order. After that point, the pizza party seemed a lot further away. When my doctor brought my family in, he wasn’t sure what he was looking at; the blood tests were inconclusive, so he explained a biopsy would help find the culprit. I was twelve, and it was 1999; Biopsy was the standard still, and I was more excited that this Saturday I would get to watch more than my allocated 30 minutes of cartoons. They’d decided to biopsy my liver, spleen, and kidney because they weren’t sure where the internal bleeding came from, and my platelets were fine. Although I had no idea this was happening, I was more focused on the McDonalds at the entrance to the hospital and the potential for Chicken Nuggets.
My follow up appointment in September made all the chicken nuggets, pizza parties, and cartoons seem entirely irrelevant. The doctor explained to my family and me that I had Hepatitis C (HCV), which was unusual for a 12-year-old, so they tested the rest of my family. The doctor also explained that because of how the disease progresses, and that I likely had it since birth and that by 30, I would need a liver transplant or die. I am glad that he was serious in his explanation and that he didn’t hold back any information. At that time, there was no cure for Hep C; there was a sliver of hope, though through a life-altering treatment. When my family’s tests came back, we were relieved when my father and brother tested negative for Hep C. But it had confirmed the doctor’s suspicion that my mom was the source, as we had the same strain of HCV. My mom was devastated, I didn’t understand how to feel. I knew that I was 12 and that I was potentially already at the midpoint in my life, so my goals and dreams faded. While there was no cure in 1999, there was treatment with a less than 30% success rate. The treatment required a year of thrice-weekly injections and a series of pills. Non-PEGylated Interferon and Ribavirin, when she took them, my mom began acting almost bipolar in her characteristics. It was hard to understand what she was going through for any of us. But Interferon essentially makes you feel like your worst flu, a dozen times over, and ribavirin can encourage emotional swings, skin issues, and both enhance fatigue. My mom made it through nearly ten months before the treatment failed her. It took years for my family to recover, but there wasn’t much time for that. She found a new job, and I entered High School. My dad had made an agreement with the school to preempt anything they may do: they would pull me out of all sports and any sports teams, and I would be barred from joining. Which meant leaving Tennis, Swimming, Wrestling, and Basketball behind. I didn’t know to talk to others about my Hep C, so I freely explained my circumstances to everyone I knew. I didn’t know that faculty and parents would react so negatively to something which could affect them in no way except their own misunderstandings and fear.
I was lucky in a way; 2002 happened to be the year a lot more people learned about Hep C. Mostly through gossip and rumors regarding Pamela Anderson and her former relationship with Tommy Lee. She was infected through a tattoo needle, although her status as a sex symbol meant that kids my age assumed it was a Sexually Transmitted Disease/Infection. By then, I realized I should be more selective with whom I share my status. My mom was ramping up for her second treatment, a PEGylated version of what she’d taken before. This version only required one injection per week but still lasted 48 weeks. This treatment would also ultimately fail her, but we still had hope it might work for me. Once I turned 18, I was given the option to take that same treatment, but I wanted to wait for better timing with school because I’d seen the debilitating state the treatment had left my mom. And as the magnet on my fridge reminded me: When you miss school, you miss out. So I waited until my senior year of college while in a long-distance relationship with an unsupportive fiancé. She wanted me to move out to Florida as she’d done nearly a year before, but my decision to treat while living with my family and having friends nearby turned out the be the best decision I could have made. She was resistant and frustrated with my choice, and it was made because I knew what I would go through; I knew the risks. I also knew that when I graduated, I could lose my health insurance, so it wouldn’t be covered otherwise until I got a full-time job. And even then, it would be a preexisting condition, so it became even more complex, and all of this was lost in our arguments. The stress was unreal, and the treatment I thought I’d prepared for was worse than I could have imagined. For three months, between my hormones pushing me to cry at doorknobs and the daily fatigue having me miss work for the first time, I was in pieces. I walked with a cane because my legs were weak from the injection sites; I used a megaphone to speak to the kids I worked with because my voice would go. I tried my best to stay in a doomed relationship, which my treatment’s failure would ultimately help me realize that maybe we weren’t right for each other. When the treatment failed, I was crushed. I didn’t know what to do; my mom was equally devastated, having hoped that maybe it would work for me, that maybe her pain wasn’t pointless.
With the help of my kids in the program I worked at, of my friends that summer, and my family supporting me, I found renewed purpose. I hit the gym, I reinvented myself, and after a few months of exploring my budding identity, I found some peace. Two years later, my doctor would suggest that I try the treatment again, only with a higher dosage. This was an unnecessary treatment. It was a year before the first Direct Acting Antivirals would come out. He was more interested in pushing the treatment because he was working for the company that made it. I learned of this years later thanks to OpenPayments, a searchable database of payments doctors receive. This was the beginning of my life with cirrhosis. Just as you’d imagine, the treatment was a bit worse than my first, and equally devastating when my viral load stayed at 3 million.(Viral load indicates the viral quantity but not the severity of illness, below 500k, is low, 500k-5mil is high, and above 5 mil very high.) I was a wreck, and my behavior and choices reflected my depreciating attitude about life. But I put myself back into again, hit the gym, reinvented myself again, and started running a before/after school care organization.
That next year, my mom would go on the single roughest treatment either of us would take. The regimen called for 3 months with the new DAA, and then 6 months additional without it. It was dubbed the triple cocktail, an ironic name as this was for liver disease. Interferon, Ribavirin, and Incivek would ravage my mom’s body requiring multiple units of blood and Procrit to keep her alive.
Ultimately she would find that her hell had paid off and was cured on her third treatment. While the Affordable Care Act had recently been passed, its stance was shaky, and I was worried about my preexisting condition preventing me from accessing insurance. And so, in the two months between when I turned 26 and my new tech support job’s insurance kicking in, I opted to fork over half my paycheck for two months of COBRA.( Consolidated Omnibus Budget Reconciliation Act Insurance can be used when employer health insurance ends for an individual, although it’s quite costly since a person pays both the employee and employer share.) Then I prepared for what I hoped would be my last treatment. I worked out for months prior, ate healthier, and tried to make the only factor that poorly affected my health, the virus. My new friend, at the time, who is now an RN, walked with me through the rough of it. My friends helped me deal with the unusual requirements of the treatment. I was to eat 10 grams of fat with each pill, which is rather hard when one has no appetite. So I’d stuff my face with crumb donettes while taking my pills, or a handful of nuts, depending on which was available. The treatment was twice as hard as anything else I’d taken previously, and it would bring me to the floor in exhaustion. I remember using a good deal of FMLA that year, so much so I’d been missed out on multiple promotion opportunities. Family Medical Leave Act allows for up to 12 weeks of unconsecutive unpaid time off. Three months after I’d started my third treatment, I found myself in a hospital ER asking for a puke bucket. Not a few seconds later, however, missing the bucket altogether, but thankfully the floor would catch most of the nearly two units of blood that projected itself from my mouth like a font. The next few moments were a bit hazy, but needless to say, they gave me an express pass to a bed; I skipped the whole ER line. They began the process to infuse blood and figure out where the internal bleeding was coming from. Had I not recognized the signs from a previous hospitalization, I’d probably have bled out even more en route to the hospital and likely died.
This was the beginning of my symptoms regularly manifesting, as prior to treatment, I’d received a MELD score, indicating the need for a liver transplant. A Model for End-stage Liver Disease score is given to patients awaiting liver transplant to show their imminent need for transplantation; the higher the score, the lower chance of living the next six months and the better chance at receiving a transplant. I was creeping closer to thirty, so my diagnosing doc’s warning was ringing in my ears. This failure was hard to accept, but like the others, I reassessed my life. I decided to leave my new job in tech support and return to working with kids. Unfortunately, over the year, I was building up my strength; my liver disease was making up for the treatments I’d been doing. My legs began to swell and retain fluid, an unusual manifestation of ascites; I’d been diagnosed with every symptom which comes with end-stage liver disease.
Hepatic Encephalopathy was the trickiest one, and one who helped get me relieved of the field I’d just reentered. Without daily lactulose, I could get trapped in mental circles mirroring dementia. My inability to do basic math proved challenging, but by using an excel spreadsheet, I felt I could compensate. My new job, however, came with new problems. The problem wasn’t my health; the problem was that I wasn’t who she wanted to hire, so they told me I was the best candidate they’d seen and was welcome to reapply; however, this position was determined to not be a right fit. The entire time I was working, she’d used my health as an excuse to push me out, encouraging me to take sick days during my evaluation period, planning meetings on days where I had appointments, knowing all of this would hurt my chances to become a permanent employee. After being let go, I was beside myself. This was the field I’d learned so well that they would ask me to come back as a consultant to help improve floundering sites. It was December of 2013, and I realized that my trajectory would have me disabled in no time. So we began the paperwork, and then, seemingly out of nowhere, something extraordinary happened.
A new treatment came out, one with a 90%+ efficacy, Sovaldi. For the first time in my life, I had real hope. I pumped up my advocacy efforts and began writing for HepMag at the invitation of Lucinda Porter after she’d read my heart-wrenching story submission and subsequently my blog I’d started during my third treatment. The treatment had to be off-label and combined with another DAA called Olysio; the combo was the first treatment to bring me to a zero viral load. And not only that, it had almost no side effects; it was life-changing. My family and friends were excited for me, but this isn’t it. This isn’t the good part. It’s not even close. It was a high moment, where my family and friends enjoyed a month and a half of knowing I would live beyond thirty and maybe have a more typical life after I hit SVR12. These treatments all have a waiting period for when one can be cured. Because it takes time to know if the treatment has been effective. That date is called Sustained Viral Response at 12 weeks or SVR12. I never hit SVR12; in fact, not six weeks later, I was hospitalized for Clostridium difficile colitis (C.Diff.) The infection I’d acquired at a diner gave my remaining Hep C the chance it needed, my jaundice was so bad, my eyes were golden yellow, and I was bumped up on the transplant list. I spent the week at the hospital, wondering when and how I would leave. The idea of a transplant scared the hell out of me even though I knew it would ultimately save my life.
Two days in, they explained that my Hep C had returned. I wasn’t allowed to leave my room alone, but thankfully I had lots of friends and family come to visit. Even an old co-worker I hadn’t seen in almost two years heard about it and stopped by. Also, coming into the hospital with C.Diff is awful, but as I was spending a week there, at least I got my own room. I also wanted to confuse the CNAs, so I had everyone bring in stuffed animals and “congrats on your baby” things because humor is excellent medicine. Upon discharge, I was informed of a new treatment and was slotted to take it by the end of the next month in November. It had a higher success rate than my previous treatment at 98%; Harvoni also required 24 weeks due to the extent of damage done to my liver. But it was just as successful as the prior treatment; by six weeks, I’d hit zero, and I’d maintained it up until May. Then, as we prepped for the annual Liver Life Walk, I received the news that my last week on treatment, the virus had rebounded, and treatment failed again.
The walk was challenging, and my body started to have trouble dealing with the symptoms, even with the medication. The cascading failures put me into a deep depression, and my girlfriend-at-the-time felt equally depressed. Months afterward, our state degraded to an untenable point; the breakup, though, was fuel for change. Sometimes it takes a kick in the head to see a different perspective, to push someone out of a funk. I redoubled my efforts, crafted a routine to help me maintain my strength and fortitude, and told all of my friends to help watch for my HE symptoms, to tell me when I should take lactulose to help ease it. I jumped back into life and began searching to find out exactly why the treatments failed and see if any treatments could match my specific situation. I found the particular mutations and why my treatments didn’t work, so I proposed a combination of two treatments, combining Zepatier with Harvoni. My doc took it under advisement, but before anything could happen, my liver hit the point of no return. As my transplant doc described it best, my liver was an old shoe, and it needed to be replaced before I could go on another treatment. My three-year wait for a transplant had, so far, gone without a call for a full, healthy liver, so I knew it would be a challenge going forward. To keep my mental faculties and physical state intact, I followed a friend to dance class. There I found the perfect outlet to work around the temporary memory loss caused by HE by introducing muscle memory to my memory castle techniques for memorization. Dance was at my own pace. I kept a bag of intentionally chosen mixed nuts (the combo helped balance my electrolytes, which would constantly be a wreck because my body would purge the retaining fluid or expelling fluid from diuretics.) Dance gave me a lot of my world back, but as my jaundice became impossible to hide, sunglasses at night were harder to pull off. I started working with a newly formed coalition of nonprofits called CalHep and helped them pass a pilot program by speaking with the assembly subcommittee. I was committed to ensuring that no one else should go through the hell of end stage liver disease because it was unnecessary if they can get treatment. At that time, there were restrictions on access, so that you needed to be F3, which is when permanent liver damage begins, to start treatment. F3 is the third tier in the liver disease fibrosis scale; F4 is usually when MELD begins. While the F3 requirement is no longer the case in California, other states like Texas (at the time of this article’s writing, Dec. 2020) still have these heinous restrictions. As an advocate, I dedicated myself to helping in the fight to the best of my ability. But in September, I began a series of monthly hospital visits, which could eventually lead to my death or maybe a transplant, and everyone around me knew it. It was the most intense period in my life, and it also happened to be October of 2016.
So everything was becoming politically charged, and tribalism was making the fight for healthcare even harder. In September of 2016, I moved along with my friends from the apartments we’d lived in for three years into a four bedroom house. It was nice, and I’m thankful that my friends were able to do this with me, especially in the condition I was in. But in my shape, setting up for the move was hard, and during the process, I passed out while explaining, “no, I just need a double-double from In N Out.” What I didn’t realize is that the craving came from a complete lack of sodium in my body. In addition to that, I happened to be Hypocalcaemic, so when I arrived at the hospital, they quickly assessed the situation and were more surprised that I wasn’t in a coma, based on how low my sodium was. I spent the week in the hospital recovering while my friends packed up my remaining things and moved me into the house. When I got home, I started to organize my things and pack for a trip. My mom had decided that we should take a cruise ship to Mexico, so she invited me and even paid for a friend to come along. I understood why she was doing this, she wanted to have some good last memories if things should come to that, and she wanted me to have some enjoyment in this rather literal hell. But that’s not in keeping with the buzzard’s luck I seem to have.
The trip was made more challenging by an odd bit of advice. Counter to literally every other doctor I’ve had, the attending doctor, during my last trip to the hospital, told me that to beat Hepatic Encephalopathy, I should really be consuming less protein and more salt. (just so we don’t spread this around, that’s TERRIBLE ADVICE, it’s the exact opposite of what should be done, low salt, high protein is correct.) But the thing is, when you have HE, memory is a tricky and confusing thing, so I followed his advice for a few weeks, including this trip. Needless to say, I looked straight up pregnant, my ascites were such that my stomach actually started to hurt on its own, and I spent most of the trip vomiting and walking in circles to avoid leg cramps because I didn’t pack my mixed nuts combo. When we returned from the trip, I found myself in so much pain, I couldn’t bend down to put on socks. The trip to the hospital had become so routine, I prepped my doc en route and told her what was going on. She confirmed what I’d suspected, I’d need a peritoneal tap. A peritoneal tap is typically a needle in the abdomen which drains excess fluid. Thankfully they were ready for my arrival, and they rushed me into triage and started work right there and were concerned. The reason for the concern was that peritoneal fluid can become septic if left for too long. And the pain was indicative of just that: sepsis. My heart rate was such that the only pain med I could take was Ketamine. As they drained twelve pounds of fluid from me and placed an Internal Jugular port in my neck to administer antibiotics in an attempt to knock out the sepsis. I was lucky that within 18 hours, the antibiotics were working, and I could slowly get better. This event had also raised my MELD from 26 to 35. I remember sharing my journey with every doctor who came in, explaining that should I live, I would get an Master’s in Public Health so that I might do more for my community. I shared my journey for two reasons, to remind myself of my purpose and to curb stigma. My higher MELD meant it was more likely that I could get a transplant, but I would wait and be denied not one but three potential transplants while the election day would frustrate my television set in the background.
Going home with a PICC line in, I didn’t know how long I’d have left; I felt better, but I knew it was relative. A Peripherally inserted central catheter line is a soft tube that goes in the left arm, allowing drugs to be more easily administered to the heart. I’d accepted and come to terms with my death should it come to that. I dug hard into my routine and got back to focusing on surviving, and waiting. I had had over eight viable liver offers at this point, and each time, renewed life was given to another person higher on the list than I. When you get to where I had, being called in for a liver offer is a regular occurrence, actually being the recipient however, is quite rare. The reason this happens is to make sure the liver goes to the person of most need where the liver and recipient will have the highest chance of survivability, they prep the top few contenders for transplant for every newly available liver.
About three weeks later, on December third, 2016, I received the call for my transplant. That day is one of the most vivid blurs because only shortly after I arrived and cleaned up, I was prepped for transplant and put under. Five hours later, I was out. Everything had gone right, and within two days, I was farting! Okay, yeah, I get it, it doesn’t sound impressive, but it’s the first step in knowing that everything is hooked up and working correctly.
Within three days, I was out of the hospital and kinda walking, I had to do a rollout method to get out of bed, because well, my abs were cut in half, but one adjusts. I was back on the elliptical within the week and ready to get back into life. My friends and family all wanted to visit, but everyone had to wear masks and gloves because of my fragile immune state, and no one who was sick could come over. Once ready, I returned home and prepped for the next step in my recovery: treatment, again. Because if this treatment didn’t work, the virus would infect my new liver, and I would be reliving the last three years of my life as my new liver slowly failed. But thankfully, my doc expanded on what I’d suggested a year earlier, prescribing me twelve weeks of Zepatier, Sovaldi, and Ribavirin. An off-label treatment was designed to target my specific variant strain of HCV. It was approved by insurance (every previous medication had been denied and required multiple appeals to push through, but this one was on Medicare.)
It, too, had its bumps as insurance goes, as I didn’t zero out until eight weeks. My team was concerned I might not reach SVR24 because four weeks isn’t a lot of time to stay a zero viral load while on treatment when you have the history I do. After weeks of stressing, calling lawyers’ offices, and preparing for a large lawsuit should it need be done, I was relieved to get to SVR12, I wasn’t quite cured, but it was a good sign. Then, 18 years after my initial diagnosis, I was cured of HCV; in early September of 2017, I reached SVR24.
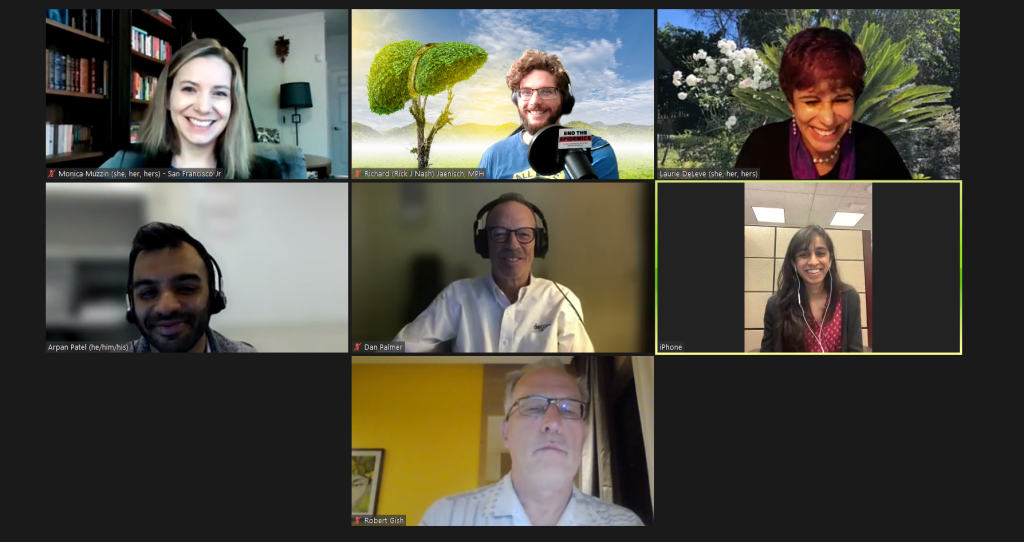
In 2017 I was already writing for HepatitisC.net, working with CalHep, the American Liver Foundation, and HepMag.com, but I needed to do more. In 2018 I started working with Help4Hep as a Peer Counselor; I stepped up at HepatitisC.net as a moderator. I stepped up my volunteering, speaking with ALF and Lifesharing, doing TV interviews to promote organ donation. Assisting CalHep in attempting to expand the pilot program I’d helped promote in 2016, and at the close of 2018, I was offered to be the Chair of the Consumer Committee at Eliminate Hep C San Diego. In 2019, I advocated with End The Epidemics and helped secure funding for HCV, HIV, and STD programs in California; I also started with a brand new nonprofit. Having been a patient advocate and a part of NoHep 2030 since it started, I knew that the goal is near impossible given our current prescription drug and healthcare system. This is why I started working for this new nonprofit, Open Biopharma Research and Training Institute. I realize that the prescription drug marketplace has many holes that increase prices, and one of those holes is manufacturing training, as there are drug shortages and lost development costs. So in an attempt to help smooth that process, I jumped at the chance to join Open Biopharma as the Director of Education and Outreach.
While preparing for the nonprofit’s launch, I finally began my Master’s in Public Health program on my third attempted application. I dove right in, researching and doing my first literature review on young people with Hep C. That Literature Review helped me craft an article that informed and encouraged others to comment on the new CDC recommendations for Hepatitis C testing. Every aspect of the new recommendations was adopted, and additional guidance reflected the research recommendations in my article. Additionally, End Hep C SD was officially kicked off in a unanimous vote by the San Diego County. It was terrific seeing advocacy work pay off, but by thesis working with HCV was muted by the arrival of COVID19. The project I’d intended on working with could no longer happen, so I dove into research on COVID19 and have since begun a systematic literature review as I am now in my final semester of my Masters’ In Public Health Program. Over the summer, I helped design health promotional material explaining the different SARS-CoV-2 antibody tests. Splitting my advocacy focus between COVID19 and Hepatitis C has been necessary. Those who are newly infected with COVID19, and COVID Long haulers, are not alone in their plight, and those of us in the HCV and HIV/AIDS communities who understand their fight have stepped up as well, like with COVIDhealth.com. We’ve already shown that when we fight to end multiple epidemics, we can sync up those fights. I look forward to graduating with my MPH in 2021 and publishing my journey with help from friends and family as a book in 2022.
2021 was a year with much promise, although January brought new challenges I’d in no way considered. While I’d extended a semester to have better time for my literature review on COVID-19 for my MPH, a new diagnosis of an auto-immune disease in my family established what we’d suspected the past few months. In the future, I’ll talk more about this, but it’s not my story to tell, although I am part of it, time will reveal all things.
In February of 2021 I was able to join the NVHR to educate and encourage the federal government to properly expand the budget for viral hepatitis to a reasonable level. (because currently it’s underfunded to an exceptionally poor degree, and at its current funding level is not capable of meeting the goal of NoHep2030.) Our hill visit also sought to improve funding for efforts regarding the opioid crisis, neither received the budget appropriate to the scale of the problem. It was an exceptional failure of vision of our congress and executive during the most significant perpetual reminder of the importance of control, surveillance and mitigation of deadly viral infections in decades. Although the experience of so many virtual hill visits was exciting and compelling, it would have been nicer if the asks were considered. In March I created an art series called the Patient Emotional Word Art Series, it ran for a little over a Month, ending before May to usher in Hepatitis Testing Month. I also launched and started guiding folks through the Socio-Ecological Model Grounding Exercise.
I’d also spent the bulk of my time preparing my defense, while my initial thesis Chair had was out sick, and I was not informed for a month, which added to the stress, I’d managed to successfully defend and Graduate in May 2021. Graduating was an amazing experience, although it still feels unreal, as I actually walk in May 2022, as I was unable to vaccinate until July 2021. I had to observe the data to see how the vaccine worked for folks with solid organ transplant like myself, and I wanted to meet with my doc before getting the Jab. I wrote a bit about my experience during this time.

Over the next few months I’d use the SEMGE alongside a built lecture and speaker series to create the Patient Advocacy Module. An teaching module of an overview of patient advocacy, all its components, designed for folks in Cell and Gene Therapy. The module was rolled into our CIRM training as it fit perfectly with the goals of CIRM. I plan on expanding the module into a week long course by next year, and some day, a full semester class.
It’s been over two years since I’d last update, due to some complexities I’ve taken a moment to be comfortable sharing in full publicly. As I learned long ago, it’s best to talk about scars, not open wounds.
Working at Open Biopharma has been great, we’ve expanded significantly in the past two years, and I’m excited about growing the patient advocacy elements and shoring up a talent pipeline for biopharma manufacturing with Mira Costa Community College. But in 2022, my life changed quite a bit. First off, In February of 2022, I got married to my amazing partner Niki, it was a gorgeous day in Cardiff, we couldn’t have asked for better weather. Given it was still during the COVID health emergency it was a small party, and we had to postpone any honeymoon.
While my MPH was now firmly behind me, I decided, I needed to hop back into advocacy as best I can. Between work and volunteering on a few local Life Sciences industry professionals boards for a few years, I’d decided I could take on another new board seat, one I’d been interested in for some time: working with the Liver Coalition of San Diego. It was great, now representing my local group when meeting with Senators and members of congress about Viral Hepatitis Elimination goals. In 2022, working with End The Epidemics, LCSD, and NVHR meant multiple avenues to help impact Policy on a local, state and national level.
I was also looking forward to the conclusion of the Craven Task Force, an endeavor I’d joined, only to find that I’d be the lone Alumnus on, as many couldn’t accommodate it’s arduous schedule, and understandably for some, the threats of violence from some in the community were too much to bear. The Task force had extended almost a year longer than anticipated, and our charge was to present informed information to the board for the final decision, so we didn’t have the power many in the community had assumed. But it was an eye-opener, learning about the history of not only the land that CSUSM sits on, but of every individual involved in the creation of the Campus as more than just SDSU north, was incredible. It also took hundreds of hours of listening to every community member who brought forward their thoughts. After learning everything we had, and discussing it at time ad nauseam, My recommendation to the Task force was to honor the history that we’d learned, to change the murals to reflect that and to make the bust of Craven part of that story. To explain to everyone who walked through those halls, the whole history from each perspective, instead of continuing the hyper focus on two individuals: William Craven and the other being Cesar Chavez, who had nothing to do with CSUSM directly, but represented well the historical roots of the community. I was a voice among maybe 20 or so folks, and the governing board made their choice to remove the name a few months later, and its now called the Administrative Building.
It was an eye-opening experience into how some task forces that involve private and public members work, and a stark contrast to the other task forces and private-public partnerships I’d been a part of. While it was well managed, well informed, it also had more opposing extreme positions than I’d encountered. Threats of violence however had become more familiar generally, due to the surge of online users, rampant misinformation, and growing animosity towards Public Health measures among a small but vocal group of people. The other big task force I’d been working with, had finally transformed fully into a Task Force: End Hep C San Diego. Given that LCSD had taken over as convener, I was in as often as I could be. Slowly we’d built good frameworks for engagement opportunities and had been trying to weather the storm of the last years of the pandemic, to figure out the how/when of holding in-person events.
Unfortunately I was not able to walk at graduation in 2022, despite what was promised to me by CSUSM officials when I spoke to them about it in 2021. I had hoped that my Grandma could have seen it, as she passed not two months later. The drive up to San Mateo, where she’d been a City Council member, Mayor, and helped open the door to Asian Businesses, banks, established green spaces laws, and even earned congressional recognition for her actions, it was also where my mom had grown up. The service was modest, family only. I did not know yet, of what challenges would lay ahead, but the next few months, my mothers health had begun to have some inconsistent challenges. This didn’t stop her from enjoying the end of 2022 and as she loved, going on cruise ships traveling around the EU and the UK.

Another advocacy opportunity came to me via email, one I couldn’t turn down. Working with a large company on an Institutional Biosafety Committee that was focusing on regenerative medicine. It was a chance to understand and meaningfully participate in a periodic meeting that would help establish benchmarks where few regulations and guidelines are currently set. Each session would be more interesting and helpful, I’ve been able to leverage my lived experience and knowledge of biopharma manufacturing, patient safety, and patient ethics.
While 2022 was coming to a close, I was also able to join in Center for Applied Special Technology(CAST) and receive Universal Design for Learning (UDL) training. This purpose of this training was to enhance the accessibility of our laboratory design. Since taking the course, I’d applied a few dozen small applications that have made big differences for everyone who comes in, and especially folks who need those adaptations. Among other things, Live transcription capacity, audio timing, big text clocks, and incorporated transition music have been practical and useful tool. But 2022 would end with more illness in family, between COVID at my parents house during Christmas, some new challenges with both my partner and I’s health, our dog having a cancer scare, then kidney nephritis, it was difficult to manage.
2022 has nothing on 2023.
Starting in January managing our dog’s toe removal surgery was made complicated due to the frequent fluid he’d need from the Kidney nephritis from contrast fluid. What we’d thought was cancer, was just an insanely arthritic joint, so his recovery was just challenging due to his growing lack of bladder control as he aged so diapers and frequent late night trips were built into our routine. He’d also stopped eating his regular food, so I’d prepare him chicken, sweet potato and rice, every day. Naturally, balancing the time demands here became intense, and while I’d dropped caffeine years ago, it came back into the picture to handle the lack of sleep.
At work, we’d made one of our biggest events yet, and it was to happen a few days after my birthday, it was months of planning, and coordination, but it was an amazing opportunity for both Open Biopharma and Repligen, the company who’s road show we were hosting, we’d also aligned a student day that was well attended by UCSD and Mira Costa Students for wet demos.

My volunteer work on the boards I was on wasn’t helping my lack of free time, working and volunteering as much as 60-80 hours per week, but I was making some serious headway, and building a foundation for future success. My birthday dinner was bookended by some unfortunate things, I’d gotten a inguinal hernia that day, which made supporting the intense week and events, that much harder. My mother’s health had also begun to decline and would soon learn she was developing ascites, something I was Intensely familiar with. So we ate indoors, for the first time in years. This meal is a complex moment, because I would not know it yet, but it would be one of the last we’d share as a family. This was compounded by the fact that both my wife and I were hit by a post viral syndrome that heavily impacted any of our existing injuries. While the meal was good, the week following the Road Show, I’d visited my mom in the hospital. The ascites had become intense, and she needed her pararenal cavity to be drained. Following her drain, they’d noticed some problems with her liver, at the time the new pressure and pain was assumed to be side effect of a weakened portal vein. It was helpful that her attending physician is a friend, colleague and even of my own medical team. It was a somber moment being on the other side of the hospital bed, in a room I’d been in not 7 years prior. I did not yet understand the scope and scale of what was ahead.
The next week, I was attending a conference on international women’s day in the OC, I’d got a ping from my partner about our dog, he’d fallen and was acting a little startled. We’d seen this happen a few weeks prior, but he shook it off in a few hours. His paws had been getting dry lately, so sometimes he’s slip, we’d remedy this with some coconut oil, and he’d bounce back with no issue.
When I got back that night he started making some strange noises, concerned, we comforted him, and reached out to my partners mom, who has extensive experience working with dogs in vivariums for advice. On the call though, I’d noticed his lips changing, and his breath weakening, he’d managed to get onto the couch with us, as we began calling the emergency vet and were preparing to take him there. The suddenness of lifting an 85 lb unconscious dog, not two weeks after being diagnosed with a hernia, was difficult and terrifying for multiple reasons, but I was able to lift him into the back seat, and I kept comforting him and keeping him warm as we drove to the Vet.
Once there, the team was ready for our arrival and helped us take him out of the car and performed emergency surgery right there in front of all of us, as her mom had joined us. They were unable to resuscitate him, they’d explained that his heart was bleeding, and even if we had gotten here earlier, he’d have only had a matter of hours at best. The reality was that he likely passed on the couch he so loved. We had our last moments with him that night.
The next day, we’d already had plans to celebrate our one year wedding anniversary at a spa, but the mist-rain that day was welcome, to have kept our day as solitary and reflective as needed. Unfortunately, later that day my discussion with my parents about my mom’s health wasn’t entirely clear. While we walked our old walks without our dog, and reflected upon his life, my dad would reveal what he took from doctors office visits alongside my mom. After the funeral for our dog, we’d learned of my mom’s new diagnosis, and the reason for the ascites: Cancer.
Health challenges were nothing new to us, so we prepared, and took this on the chin. We picked up every tool she’d need, I was preparing to take as much time off as needed and my brother was going to fly down to help. That Easter my mom tried her best, she’d undergone her first round of Chemo and was having a hard time even speaking. Her ascites had gotten worse, and I’d asked my dad why she wasn’t getting regular taps to drain it, but her oncologist didn’t think it necessary. She was able to join us for a punctuated Easter, and spent the remainder in bed. We spoke for a short time about what lay ahead, and the plans we could have to make it through. She’d asked about how my ribs were feeling, as the post viral syndrome had been causing an intense arthritic flare in my sternum, the formerly broken from my liver transplant.
Monday Morning, I received a frantic call from my dad about my mom being in the ICU at a local hospital. It was painful to lean over her bed for as long, but I was there at each rounds and then some, the benefit of the hospital being 10 minutes drive away. It was difficult attempting to work at this time, but I couldn’t abandon what I had been building to. Each day I’d spend more time at the hospital, trying to minimize my own health exposure, as well as manage the pain. On my way to the hospital I’d put on a playlist that began with Paramore’s Hard Times, as it rang familiar during my own brushes with death in 2016.
As the days progressed, her state began to worsen, my brother was on his way from Oregon, and prepared for an arrival on Friday Night. She was constantly surrounded by a medical team, as her cancer was aggressive and few solutions were able to treat the sepsis, she refused paid medication, day after day. Something I knew could not have come easy, she wanted clarity as she knew an important decision might come soon. Her voice becoming more and more faint as her lungs were unable to fully inflate, her diagram under pressure from the ascites, she was given an asperation spirometer. The tool I’d used to monitor and train for months to get back from my own bout of sepsis. I’d walk her through her use each day, and her last words with her own breath to me “You Encourage me” a harder to swallow pill, when I’d receive a call not 24 hours later that Friday afternoon. She’d asked for me, to help make her make the choice to die peacefully.
Calling my dad, and brother, we’d arranged what we could, and my mom passed peacefully later that night. We were with her as long as we could be, my dad stayed until my brother could get in late that night.
It remains one of the hardest moments in my life, but one I understand well, as she and I have often talked about death. Prior to my bout of sepsis, I’d had other brushes, and I recall explaining to her that if my time should come, know that I’m at peace with this. To reflect this stance a little more than seven years after my life-saving transplant, I was glad for the time we’d had together.
Needless to say the next few months were a wave of conversations, therapy and lots of walking. I’ll always live by my creed Solvitur Ambulando. I’m glad for my partner for her grace, and for our time to reflect together, for my friends and family for rallying around one another to get through this together. The memorial was an emotional journey in and of itself. My brother’s decision to move down here came shortly after, some epiphanies and important new realities fed this. Our dad appreciated the extra family time. We’d adopted a new dog, which in truth was a lot of work to reestablish our new bonds with. The hernia, it turns out, can’t be operated on, as the risks for me are too great, which took four months, and four specialists to find out for some reason. The post viral syndrome took months to fade, and the gabapentin I took to help relieve the pain was actually making it worse, as long term use can cause chest pain, the two were confounding with my grief to become particularly difficult to work around.
I took a month-ish off bereavement to do the many things needed for recovery, but by June, I was back at it, advocacy was challenging, but I was able to still join for virtual hill days. It was essential as Biden had announced White House involvement in the campaign to Eliminate Hepatitis C and joining NoHep 2030, although with a more realistic timeline.
(Also…It’s very frustrating that we use the 2.4 million number as people with HCV in the US, since that data point is from a Literature review collected about a decade ago, and the number is likely higher, as that was an underestimation. Fun Fact: the CBO recently ( June 2024) provided feedback on the effort, and largely it looks promising. )
At work, I’d started a ChatGPT project in part as a distraction, in part because I felt that education was looking at ChatGPT in the wrong way, and understanding these tools would be essential in the years to come.. The first round of the parallels project began that Summer, and it provided a lot of direction on how to change the project for the next cohort. The workshops came and went successfully again, featuring a solid afternoon of patient advocacy and a Patient Advocate colleague of mine Dan Glass.
The strange empty feeling of my mom’s void, soon became a driver of doing well by her memory. Reminding myself to strive to be as great as my mom believed me to be.
My brother and I knew we needed to make something of the year, make something from this grief, do something beyond where we’d been. So David and I sought again to build a company, Generative AI seemed to be a practical consideration, not six months ago ChatGPT 3.5 had become the fastest app to reach 100 million subs, and there was a lot of potential for the tool. At first we’d thought education might be the best aspect, as these tools can lead to rampant misuse, and can be dangerous in the wrong hands. But David’s skills would have languished in such a small endeavor, so consulting and bespoke tools became the primary focus as we spent the next few months, and education to support it. We’d focus the goal to being ethical, person-first, which meant focusing on the person doing the job, and letting them lead the pathway, it meant considering what limitations prevent its use among patients. It meant a lot of reading, and experimenting. It took months, but we’d found the company at the end of 2023. We’d found Prompting Integration and Consulting LLC, or PICLLC, to help life sciences and healthcare companies make ethical and practical AI integrations focused on Generative AI.
As the year came to close, I also received some good news about 2024, from an organizations I’d been following closely since I started descending into End Stage Liver Disease: AASLD almost 16 years ago. They’d selected me for the Patient Advisory Group for 2024-2026, I was elated, It was a great way to close out a otherwise harrowing year.
Each year I plan on updating my story to share as the journey continues. If anything, I hope my story inspires you to help someone close to you who has Hep C, who you may not have understood the potential for their plight, or to help yourself remind you that you have so much more potential than you know. We are all worthy of treatment, care, and love. The more we share our stories, the more we can help erase stigma.
TLDR; When it comes to Hep C: Get Tested, Get Treated, Get Cured.